Hepatitis Free Mongolia (HFM)
“Hepatitis Free Mongolia” evolved from FIRE’s “Love the Liver” program, which began in 2009 under a Memorandum of Understanding with the Ministry of Health (MoH). Since then, FIRE has supported MoH and the World Health Organization’s (WHO) guidelines and goals in preventing, diagnosing, and eliminating viral hepatitis and liver cancer across Mongolia. Hepatitis Free Mongolia is designed to fill the gaps in Mongolia’s national Healthy Liver Program and to be replicated in communities worldwide, empowering individuals and healthcare systems with the training and tools to end the hepatitis epidemic.
“Hepatitis Free Mongolia” is a collaborative, community-based model to eliminate hepatitis at the provincial level. By leveraging national support systems and the National Healthy Liver Program, the Hepatitis Free Mongolia systemically locates the missing people needing testing and connects them to treatment. The program is designed to be replicated across Mongolia and communities worldwide. We plan to scale the program across Mongolia, making Mongolia the first country in the world to eliminate hepatitis.
Hepatitis Free Mongolia, Phase 2 began in the Summer of 2021 with the goal of eliminating hepatitis C (HCV) across Sukhbaatar province while creating a scalable project for HCV elimination in rural Mongolia. As of January 2025, it has screened 94.4% of the target population (everyone in the province age 15 and older), and cured 42% of those testing positive. Please read below for more details about Phase 2.
Hepatitis-Free Mongolia, Phase 3, will begin in 2025 in Govisumber province. Govisumber has the highest mortality rate of liver cancer in Mongolia, 2.3 times higher than the second highest. This province has a high migrant population due to its mining sector, transportation hub, unique climate, and quadripoint of four other provinces.
Phase 3 is intended to quickly replicate and test the model on a small scale, looking for additional adjustments before scaling up. We will also add hepatitis B and D initiatives and expand our healthcare working capacity building with local and international training and an ECHO model.
Phases 1 and 2 were funded by Rotary International and Gilead Sciences and implemented in partnership with Rotary International and various stakeholders.
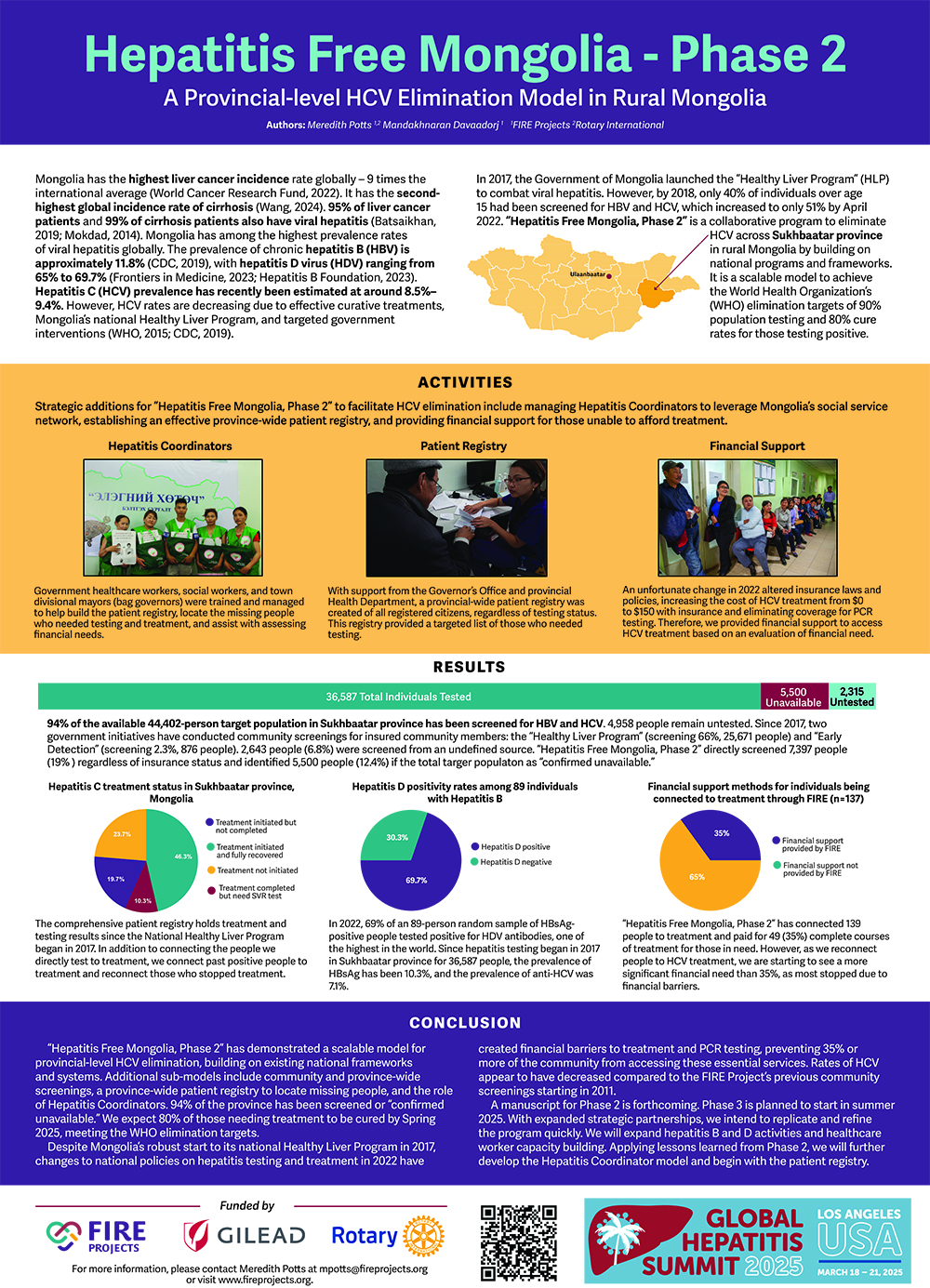
Mongolia has the highest liver cancer incidence rate globally, 9 times the international average (World Cancer Research Fund, 2022). It has the second-highest global incidence rate of cirrhosis (Wang, 2024).
Quick Facts
(since 2011)
- 15,815 people screened in eight provinces and Ulaanbaatar
- 10.4% of people were positive for hepatitis B
- 7.3% of people were positive for hepatitis C
- 64% of people were positive for hepatitis D
- 0.4% of people were positive for liver or other abdominal cancer
- 7,349 UltraSound examinations given
- 6,761 exams provided by hepatologists and oncologists
- 1,504 FibroScan examinations given
In the News
95% of liver cancer patients and 99% of cirrhosis patients also have viral hepatitis (Batsaikhan, 2019; Mokdad, 2014). Mongolia has among the highest prevalence rates of viral hepatitis globally. The prevalence of chronic hepatitis B (HBV) is approximately 11.8% (CDC, 2019), with hepatitis D virus (HDV) ranging from 65% to 69.7% (Frontiers in Medicine, 2023; Hepatitis B Foundation, 2023). Hepatitis C (HCV) prevalence has recently been estimated at around 8.5%–9.4%. However, HCV rates are decreasing due to effective curative treatments, Mongolia’s national Healthy Liver Program, and targeted government interventions (WHO, 2015; CDC, 2019).
In 2017, the Government of Mongolia launched the “Healthy Liver Program” (HLP) to combat viral hepatitis. However, by 2018, only 40% of individuals over age 15 had been screened for HBV and HCV, which increased to only 51% by April 2022. “Hepatitis Free Mongolia, Phase 2” is a collaborative program to eliminate HCV across Sukhbaatar province in rural Mongolia by building on national programs and frameworks. It is a scalable model to achieve the World Health Organization’s (WHO) elimination targets of 90% population testing and 80% cure rates for those testing
Despite seeing a reduction in the prevalence of Hepatitis C (HCV) over the last 14 years, Mongolia has remained the world leader in mortality rates for liver cancer and prevalence of Hepatitis B (HBV) and D(HDV).In 2017, the Government of Mongolia launched its national Healthy Liver Program (HLP) to control viral hepatitis. In 2018, one year after HLP’s launch, 40% of those over age 15 across Mongolia had been screened for HBV and HCV. As of April 2022, 51% had been screened. The slowing momentum for the HLP can be partially attributed to COVID-19 which left Mongolia in lockdown for almost two years, and multiple changes throughout Mongolia’s leadership.
In 2016, this project was one of five international programs recognized by the WHO and the European Association for the Study of the Liver (EASL) for “Innovative Hepatitis Screening.” In 2017, it was featured three times in the Economist Intelligence Unit for its innovation and exemplary model for HCV testing.
At each new implementation, services are added, and adjustments are made based on community needs, input, and lessons learned. The critical aspects of Hepatitis Free Mongolia are listed below.
Results as of May 2025:
94% of the available 44,402-person population over age 15 in Sukhbaatar province has been screened for HBV and HCV. Since 2022, “Hepatitis Free Mongolia, Phase 2” directly screened 19% of the available people regardless of insurance status and identified 5,500 people (12.4%) as “confirmed unavailable. Since 2017, an additional 66% were screened by the Healthy Liver Program, 2.3% were tested by the Early Detection Program, and 6.8% were tested by an undefined program.
The World Health Organization’s (WHO) definition of elimination requires screening 90% of a community and treating 80% who test positive. 54% of the expected HCV RNA positive patients have completed treatment. 20% have started treatment. We expect 80% of those needing treatment to be cured in 2025, meeting the WHO elimination targets.
Additional Activities include:
- Conducted multiple mobile screenings reaching 14 “county (soum) clinics” 2-3 times each in 2022-2023 with comprehensive liver testing
- Directly screened 7,397 people for hepatitis B and C.
- Provided 3,535 ultrasound and 1,333 FibroScan examinations.
- Hepatologists or oncologists saw 2,516 people,
- 49 people were diagnosed with liver cancer and immediately connected to specialized care in Ulaanbaatar.
- Directly connected 137 people to treatment, paying treatment cost for 49, a financial need of 35%.
- Testing results have shown:
- 10.3% positive for HBsAg.
- 7.1% positive for HCV antibody, with 54% of those being HCV RNA positive.
- In 2022, 69.7% of 89 random HBsAg-positive samples had positive HDV antibodies.
- HBsAg positivity is 11.2 % among 25-34 year olds who were vaccinated at birth within the first 24 hours.
- Trained 150 social and healthcare workers and “bag governors” throughout the project to be Hepatitis Coordinators to leverage the government’s social service network, registration system, and patient registry.
- Managed a network of 20 lead Hepatitis Coordinators to find the missing people.
Conducted advocacy meetings with community, government and business leaders selected by the Health Department to bring the community’s logistics and financial influences together to implement further solution-based programming.
Held a community fair and distributed thousands of liver health pamphlets.
“Hepatitis Free Mongolia, Phase 2” demonstrates a scalable model for provincial-level HCV elimination, building on existing national frameworks and systems. Additional sub-models include community and province-wide screenings, a province-wide patient registry to locate missing people, and the role of Hepatitis Coordinators.
In the fall of 2017, FIRE worked with the Rotary Club of Ulaanbaatar and the Rotary Club of Flagstaff to implement “Hepatitis Free Mongolia, Phase 1,” a Rotary-funded Global Grant. “Hepatitis Free Mongolia, Phase 1” visited every county and rural public hospital in the province.
Throughout this project, 5,017 people were screened for hepatitis B and C with blood tests, FibroScan, ultrasound examinations, and physical examinations by specialists in 14 locations across Dornod province. 1,966 people were vaccinated against HBV, 36 healthcare workers were trained, 20 computers were delivered, 50,000 information pamphlets were distributed, and 20 community leaders participated in an advocacy meeting.
From the total budget, 8% was saved and redirected to training healthcare workers and social workers to be Hepatitis Coordinators in Dornod and Tov provinces in 2018 and 2019. For more information about “Hepatitis Free Mongolia, Phase 1,” please view our Phase 1 final report.
In Phase 2, we developed a patient registry to track our screening and treatment progress and document reaching 90% of the target population. A comprehensive patient registry is essential to achieving elimination. In Phase 3, we will leverage insights from previous phases to implement an enhanced registry system.
Key aspects of the Patient Registry include the ability to;
- Prepare comprehensive lists for Hepatitis Coordinators to strategically invite individuals to the screening who need to be tested or who have tested positive and need treatment.
- Coordinate with the Provincial Health Department to synthesize testing status with results from other Government initiatives.
- Collaborate with local administrative officials to update the contact information of missing people who have moved out of state or the country.
- Work with primary clinics to update testing status and results continuously.
The ‘Hepatitis Coordinator’ role, conceptualized and implemented during Hepatitis Free Mongolia, Phase 1, with the support of Rotary Club of Ulaanbaatar and Saga University in Japan based on a model Saga University has been using for several years. Since 2017, 300 healthcare workers, social workers, and community members have been trained as Hepatitis Coordinators in three provinces.
Hepatitis Coordinators are government-employed social workers, healthcare workers, and bag governors selected by the provincial health department with clear roles, expectations, and compensation structures.
All Mongolian citizens are documented in a centralized national registry and assigned to a local clinic and social welfare office. The Hepatitis Coordinators work within these systems to locate individuals, assisting and advising them on the steps for testing and treatment, regardless of whether they are insured.
Hepatitis Coordinators are trained to help build the patient registry, locate and guide community members, educate the community about hepatitis, and raise awareness on prevention and treatment by visiting schools, government offices, and other places of employment.
Mongolia’s national Healthy Liver Program currently requires several tests to begin hepatitis treatment that are not available in rural Mongolia, where half of the country’s population. Some required tests are not available at the primary care clinic, meaning people can have to travel for up to one day to reach the provincial capital for the testing. Other tests are simply not available at all outside of Ulaanbaatar, Mongolia’s capital, such as FibroScan.
A team of Mongolian specialists consisting of an oncologist, hepatologists, and ultrasound and FibroScan specialists, travel from Mongolia’s capital city, visiting every health clinic in the province to provide the following free services:
Step 1: Rapid serum tests for viral hepatitis B and C are given.
Step 2: Those positive for HBV or HCV have an ultrasound examination.
Step 3: Those with liver lesions are tested for AFP and are seen by an oncologist.
Step 4:Those with signs of cirrhosis during the ultrasound exam are given a FibroScan and seen by a hepatologist.
Step 5: Those who test positive for HBV or HCV but have no indication of current cancer or cirrhosis are seen by a hepatologist.
Step 6: Hepatologists and oncologists physically examine and counsel participants on their medical condition, follow-up treatment, physician referrals, and necessary lifestyle changes.
Counseling includes an explanation of their medical condition, future care, and follow-up treatment. Patients will receive a short booklet detailing treatment options, proper nutrition, transmission prevention, and the necessary lifestyle changes they need to make. Counseling also includes physician referrals and connection to treatment.
Additional HBV, HCV, and AFP tests will be left for the uninsured at each primary care clinic. By traveling to every clinic in the province, we are providing access to testing and connection to treatment to the province’s most remote people.
The inclusion of government specialists from Ulaanbaatar provides a direct connection to treatment, bypassing months of waiting and possibly impossible travel costs.
The tools have long been available to eliminate HCV. Mongolia previously held a pioneering position in hepatitis C virus elimination efforts, setting an early example for the world in the fight to end hepatitis. Mongolia’s HLP, extensive social service network, individual registration numbers, and well-connected healthcare infrastructure create a prime opportunity to accomplish its stalled goal. This initiative exemplifies the feasibility of eliminating and potentially revitalizing Mongolia’s Healthy Liver Program and path for other communities worldwide.
Through the synergistic integration of multiple intervention strategies, working with Hepatitis Coordinators to utilize the patient registry and providing support for those in need we will eliminate HCV at the provincial level with 90% screening coverage for hepatitis C and B viruses among the population aged 15 and above, and successful treatment and cure of 80% of individuals testing positive for hepatitis C virus These activities are:
- Connect patients to treatment
- Coordinate patient care
- Provide financial support for the uninsured
- Employ Hepatitis Coordinators
- We will implement the patient registry
In addition to training hepatitis coordinators, in conjunction with our mobile screening, we conduct capacity-building activities for healthcare workers led by specialists visiting Ulaanbaatar, the United States, and abroad. Local physicians shadow specialists during the screening activities and lead additional classroom sessions. Specialists leading the training include oncologists, hepatologists, ultrasound specialists, and fibro-scan specialists. The Mongolian Ministry of Health approves the curriculum and methodology, and all participants are given continuing medical education (CME) credits for the training. For more information, please visit our Healthcare Worker Capacity Building webpage.
Community Awareness Events are conducted to support various activities, including Hepatitis Free Mongolia and World Hepatitis Day. In addition to the community awareness fair, we spend time at local markets, in schools, local businesses, and other locations, distributing thousands of pieces of information and promoting awareness.
- Distribution Awareness Materials throughout the community
- Direct Community Outreach
- Small community gatherings and outreach at local community centers, schools, and businesses
- Travel to visit remote families with the bag governor on his annual rounds
- Visiting markets and other gathering spots
- Community Awareness Fair and Opening Ceremony
- Advocacy meetings with the community, Government, and business leaders.
For more information, please visit our Community Awareness webpage.
The hepatitis B vaccine protects against liver cancer. It will be provided to everyone who will accept it. We will contact government offices, large businesses, and community markets to increase this number and offer vaccination.
The healthcare environment is one of the leading forms of transmission for infections, including blood-borne viruses such as hepatitis. Poor medical waste management, handling of sharps, and health safety practices are primarily attributed to the cause of this transmission. In future Phases of Hepatitis Firee Mongolia, we will increase infection prevention and control efforts in the clinics with supplies and education for healthcare workers, including unregulated dental clinics. We will also educate community members administering home healthcare, tattoo studios, beauty salons, and other high-risk community businesses. For more information, please visit our Infection Prevention and Control webpage.
This initiative aims to generate the following data to inform global stakeholders, including governmental bodies and organizations and stakeholders worldwide, about hepatitis program management, gaps, barriers, lack of access, and treatment issues. The eradication model developed through this project has the potential for scalability and adaptation across diverse communities in Mongolia and globally. Some of the data produced by this project will include:
- Comprehensive analysis of disparities in hepatitis screening and therapeutic interventions within Mongolia to inform evidence-based policy modifications and strategic updates.
- Further testing and development of a patient registry.
- Epidemiological data on prevalence rates for diverse hepatic disorders, with specific emphasis on hepatitis D virus (HDV).
- Detailed protocol for implementing community-centric interventions to enhance screening participation and treatment adherence.
- Comprehensive methodological framework and replicable program model.
- Synthesis of lessons learned and evidence-based recommendations for future program development and implementation.